| 3 Dec 2020 – Donation Ethics publishes its fourth open letter – more news |
 |
Donation Ethics |  |
| Ethicists and Economists for Ethical Donation Practices | ||
3 December 2020
Open letter to the Board of Canadian Blood Services Urging the Creation of a Cooperative Canada-U.S. Kidney Paired Donation Program
- INTRODUCTION
- We are professionals who work in the fields of health, ethics, public policy, and economics. Several of us have donated a kidney (non-directed, altruistic kidney donation). Several of us have experience launching Kidney Paired Donation (KPD) programs in the United States and other countries.
- Currently, there are nearly 3,500 Canadians on a waiting list for a kidney.1 In the United States this number approaches 100,000.
- This open letter urges Canadian Blood Services to commit to creating a joint Canada-U.S. Paired Kidney Donation program as soon as possible.2
- The benefits of KPD are well known. Such programs are in place in countries around the world. International KPD programs are rarer, but not without precedent. Given this, the letter’s recommendation is modest. But the benefits of such a cooperative Canada-U.S. KPD program would be substantial. Many more Canadian and American lives would be saved and improved through cooperation. It would also reduce health care costs compared to the status quo.
- KIDNEY PAIRED DONATION
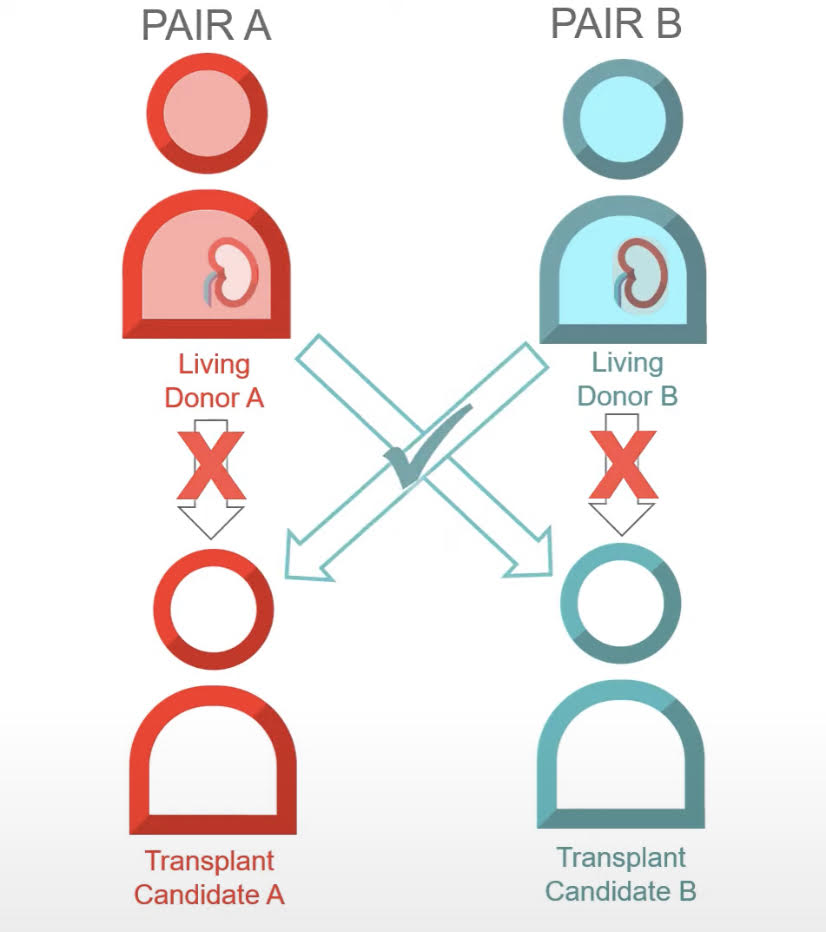
- One constraint on the number of transplants performed is biological incompatibility. Too often, those in need of a transplant have a willing donor, but not one whose kidney is a compatible match. These missed opportunities have dire consequences.
- Fortunately, many of these compatibility problems are surmountable through KPD. For example, suppose Alice needs a transplant and has a brother who is a willing but biologically incompatible donor. And suppose their neighbor also needs a transplant and also has a willing but biologically incompatible donor. It looks like both recipients would be tragically unlucky in this circumstance. However, with KPD, Alice’s brother may be a match with the neighbor, and the neighbor’s donor may be a match with Alice, thus enabling a happy outcome for all. The more incompatible pairs in the pool, the more likely it is that two will be a match.
- SIZE MATTERS
- The success of these programs depends crucially on their size. The more pairs in the pool, the more likely it is that two individuals will be mutually compatible.
- The benefit of a larger pool is nonlinear. For example, on average, with 25 eligible pairs we can expect fewer than nine transplantations. But with 100 pairs the average number of transplants increases to almost 50. If, in addition to exchange between pairs, we facilitate chains of three or four participants, that number grows to more than 60.3
- We recognize that Prince Edward Island (population: 156,947 in 2019) benefits from sharing a list with the much larger province of Ontario (14.57 million in 2019). Each enlargement of the pool of available pairs increases the odds of finding a biologically compatible match.
- Engaging in a cooperative KPD program with the U.S. would be to the benefit of Canadians who require a kidney transplant. We can expect to see more lives saved, and health care costs reduced.
- COMPELLING PRECENDENT
- Cooperative KPD programs are neither unprecedented nor unusual. As we have mentioned, Canada runs an interprovincial program. The United States also runs similar programs, both regional and national.
- International cooperative KPD programs are also not unprecedented. New Zealand (population: 4.886 million in 2018) and Australia (population: 24.99 million) have recently established such a program.
- Indeed, such cooperation is not unprecedented between Canada and the United States. Ten years ago a chain involving ten recipients and ten donors, with one pair from Canada and nine pairs from the United States, was successfully conducted at McGill University and at Johns Hopkins University.4 In 2012, Canadian Josephine Bonventre participated in what was called “Chain 124” which included 60 operations, connecting 30 donors with 30 recipients, the then-longest chain.5
- Already many Canadians join the National Kidney Registry in the United States in order to take advantage of the much larger system in the U.S. This is less efficient than a cooperative program.
- INTERNATIONAL KIDNEY PAIRED DONATION IS MORALLY URGENT
- KPD is widely and rightly regarded as a vital and ethical means of increasing access to transplants. Not only are many lives saved, but even more are improved by releasing them from the burden of dialysis. Simply put, saving and improving lives is morally urgent.
- Transplantation is also more cost-effective than dialysis. Both countries stand to save significant health care resources from cooperation. These resources can be redirected to other health care priorities.
- IMPLEMENTATION
- We can envision no insurmountable obstacles, and all are trivial in the face of the benefits of additional possible lives saved, and health care resources saved.6
- There may be political or regulatory obstacles to the creation of a cooperative Canada-U.S. KPD program. For example, customs and border regulations regarding the shipping of kidneys, or obstacles regarding health insurance coverage of transplantation. There may be technical, programming, or algorithm-related obstacles. Each of these can be dealt with on an as-needed basis.
- We commit to help overcome these obstacles, including introducing or repealing legislation, and helping to create or augment new or existing matching algorithms.
- CONCLUSION
- It is well beyond time for a Canada-U.S. Paired Kidney Donation program. There are no ethical or cost-related objections to the creation of such a program. There are only trivial, inconsequential obstacles, in comparison to the possible benefits.
- We have already lost lives and failed to improve the quality of life of too many Canadians and Americans by not instituting such a program ten years ago. Each year that we wait to create this program is another year that patients who would receive a kidney if we had such a program have to needlessly suffer.
- Given the significant and morally urgent benefits of creating such a program, we urge Canadian Blood Services to commit to the creation of a cooperative KPD program today.
Signed,*
Aaron Ancell, Bentley University
Itai Ashlagi, Stanford University
Donald Berwick, President Emeritus and Senior Fellow at the Institute for Healthcare Improvement, Former Administrator of the Centers for Medicare and Medicaid Services
Ned Brooks, National Kidney Donation Organization +
Alex Chan, Stanford University
Lisa Emmott, National Kidney Donation Organization
David Faraci, Durham University
Mark Fedyk, Betty Irene Moore School of Nursing, University of California (Davis)
Peter M. Jaworski, Georgetown University
Nicholas King, Faculty of Medicine, McGill University
Frances Kissling, Institute for Philosophical Research, UNAM
Kimberly D. Krawiec, Duke University
Chelsey Larson, National Kidney Donation Organization +
Chris MacDonald, Ryerson University
Frank McCormick, Bank of America (retired)
Ellis Mirsky, Esq, National Kidney Donation Organization
Josh Morrison, Waitlist Zero +
Peter Mpaka, Kampala International University
Luke Semrau, Bloomsburg University +
Scott Reid, Member of Parliament for Lanark-Frontenac-Kingston
Alvin E. Roth, Stanford University, Nobel Prize winner (Economics)
Betsy Caroline Snow, National Kidney Donation Organization +
Nancy Walton, Director, Daphne Cockwell School of Nursing, Ryerson University
Arthur Ward, Michigan State University +
Mark Wells, Northeastern University
1 The Kidney Foundation of Canada. Data is estimated from numbers provided for 2018.
2 We join others who have urged and recommended the same. In 2009, Dr. Jeffrey Veale urged the creation of such a program which, he said, would help thousands. “Kidney chain that pays it forward could help thousands: doctor,” CBC News, 4 June 2009. Similarly, nearly 10 years ago, a group of transplant professionals wrote in the New England Journal of Medicine: “The transplant community must act now to remove barriers to a broader implementation of international sharing of KPD lists to further optimize the potential of this modality.” Also nearly ten years ago, a team of transplant professionals wrote in a Letter to the Editor for Transfusion Journal: “KPD sharing between Canada and the United States is logistically tenable due to a shared border, language, and relatively short travel distances. In fact, a chartered flight from Baltimore to Montreal is shorter than many of the current flights for live-donor organ transport in other areas of the United States, which have resulted in prompt allograft function (7). Additionally, the American Society of Transplantation, the American Society of Transplant Surgeons, and the Canadian Society of Transplantation share close collaboration and similar philosophical understandings. It seems logical that the transplant centers in the United States and Canada would benefit by combining KPD pools and allowing more patients to be transplanted. We would suggest re-looking at this UNOS policy with revisions in mind to allow for international exchanges with centers that have regulations and mission to that of UNOS.” See: Garonzik-Wang, Jacqueline M.; Sullivan, Brigitte; Hiller, Janet M.; Cass, Valerie; Tchervenkow, Jean; Feldman, Liane; Baran, Dana; Chaudhury, Prosanto; Cantarovich, Marcelo; Segev, Dorry L.; Montgomery, Robert A. International Kidney Paired Donation, Transplantation Journal: 15 October 2013 - Volume 96 - Issue 7 - p e55-e56.
3 Roth, Alvin, E., Tayfun Sönmez, and M. Utku Ünver. 2007. “Efficient Kidney Exchange: Coincidence of Wants in Markets with Compatibility-Based Preferences.” American Economic Review, 97 (3): 828-851.
4 Canada and the U.S. have collaborated on at least one international KPD chain from September 2009, and concluding in July of 2010 at McGill University and Johns Hopkins University. See: Garonzik-Wang, Jacqueline M.; Sullivan, Brigitte; Hiller, Janet M.; Cass, Valerie; Tchervenkow, Jean; Feldman, Liane; Baran, Dana; Chaudhury, Prosanto; Cantarovich, Marcelo; Segev, Dorry L.; Montgomery, Robert A. “International Kidney Paired Donation,” Transplantation Journal: 15 October 2013 - Volume 96 - Issue 7 - p e55-e56.
5 “Longest kidney transplant chain in history had a Canadian connection,” The Star, 24 February 2012.
6 As Jay S. Connolly, Paul I. Terasaki, and Jeffrey L. Veale put it in a letter to the editor of the New England Journal of Medicine nine years ago: “These challenges are inconsequential next to the potential benefit for patients who might receive transplants as a result of internationally broadened KPD” (P. 869, “Kidney Paired Donation — The Next Step,” N Engl J Med 365:9, 1 September 2011).
* The views expressed are those of the signatories and are not necessarily shared by the institutions with which they are affiliated.
+ Altruistic, non-directed kidney donor
+ Altruistic, directed kidney donor

